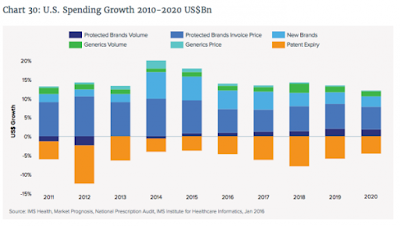
Center for Medicare and Medicaid Services New Plan to Curb Medicare Prescription Drug Price Inflation
The way the Medicare program works now is pretty straightforward: Part B pays the average sales price of a drug plus a 6% add-on. This add-on is what’s designed to cover the costs of care for physicians and their staff. But there’s the idea floating around among the Centers for Medicare and Medicaid Services, which is implementing this experiment, that physicians are being influenced to prescribe the most expensive drug rather than the best drug for a patient to garner the biggest add-on possible.
The solution? The new model, which is being tested in select markets, pays the average sales price of a drug while imposing an add-on payment of just 2.5%, plus a flat-fee payment of $16.80 per drug per day. The CMS’s idea behind this change is to see if patient quality and value of treatment can be improved while simultaneously saving Medicare money.
 |
| Source: Centers for Medicare and Medicaid Services |
Although improved patient quality and value are broad goals of the CMS, there are a few specific strategies they’re targeting. For one, they hope to substantially reduce patient cost-sharing. If physicians opt for those cheaper medications, then the consumer will be on the line for 20% of a much lower cost (Medicare typically covers 80% of qualified medical expenses, with the consumer picking up the remainder).
This experiment would also help the CMS examine indications-based pricing. The CMS would analyze the clinical effectiveness of certain therapies and, based on price as well, weed out what works and what doesn’t so the program only pays for therapies that provide positive results and good value for patients.
Lastly, this model will test the effectiveness of a standard payment rate for groups of similar therapeutic products. No flat fee has been tested like this before — but if effective, it could dramatically lower program costs.
Will it work?
The new plan is a rough draft and in time, with diligence and proper oversight, the finished product is going to eliminate incremental waste. My primary concern is the 2.5% add-on payment. The percentage basis incentivizes manufacturers to jack up prices and physicians to prescribe more costly medications although less costly yet therapeutically equivalent products are on the formulary. A better strategy would have been to add more dollars to the dispensing fee thus completely eliminating the add-on percentage. Simply put, the plan will eventually work.