With October deadlines in the rear-view, hospitals and health systems that participate in the 340B drug pricing program are scrambling to respond to a flurry of new audit demands from drug manufacturers, as well as manufacturer limitations on the number of contract pharmacies that these covered entities are allowed to use under 340B. Manufacturers and providers participating in the 340B Drug Pricing Program have entered into a new phase of tensions this summer, as manufacturers push back on the use of contract pharmacies by providers.
Additionally, beginning in June, some manufacturers sent letters to providers, directing them to upload contract pharmacy claims data for 340B-eligible prescriptions to the vendor 340B ESP to minimize duplicate discounts for claims that are submitted to Medicaid, Medicare Part D, and commercial payors. 340B administrator entities responded by sending communications to the same providers, reminding them of the confidentiality and data privacy obligations governing the claims data, and refusing to provide authorization to disclose data for payors other than Medicaid.
One manufacturer’s announced refusal to sell drugs for shipment to contract pharmacies is the strongest stance on this issue so far. This announcement will require a response from HRSA (the agency endorsed the use of contract pharmacies in a 2010 regulatory notice), which may ultimately lead to a court battle on the question whether the use of contract pharmacies is permissible under the 340B Program.
Drug companies have become more emboldened in recent weeks to restrict sales to contract pharmacies as legal experts say the Trump administration lacks authority to crack down on the drug companies. Merck, Sanofi and Novartis have called for contract pharmacies to submit claims in order to avoid duplicative discounts. Back in July, Lilly restricted sales to contract pharmacies of three formulations of the erectile dysfunction drug Cialis.
Tyrone’s Commentary:
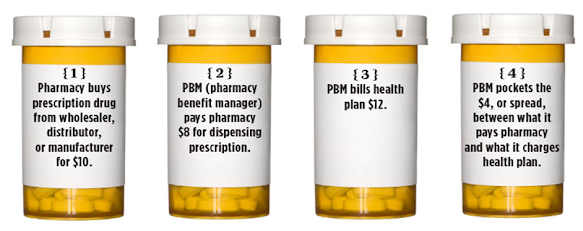
That pharmaceutical companies would incorporate more compliance initiatives into the 340B program should come as no surprise. Some hospitals were pocketing the savings from 340B discounts instead of offsetting patient out-of-pocket costs, for example. This is only the beginning. First, drug manufacturers clamped down on rebate aggregators and their submission of duplicate or unqualified claims for rebates. Now, the focus has shifted to the use of contract pharmacies by 340B covered entities. Next, I presume drug manufacturers will shift their focus to the abuse of copay maximizer and manufacturer assistance programs. There is no long-term substitute for being an astute caretaker of your employer-sponsored pharmacy benefit plan.
Pharmaceutical companies are targeting a popular tool used by hospitals in the 340B program, which requires drug companies to provide discounts to safety-net hospitals in exchange for participation in Medicaid. Roughly one-third of the more than 12,000 340B hospitals use a contract pharmacy to dispense the discounted drugs, according to a 2018 report from the Government Accountability Office.
The GAO report found that the Health Resources and Services Administration, which oversees the 340B program, does not fully assess compliance with the program’s prohibition on duplicate discounts for drugs prescribed to both Medicaid and 340B. Pharmaceutical manufacturers have also charged that the discount program has gotten too large and unwieldy.
Continue Reading >>