Adviser or Broker – which standard is most beneficial to plan sponsors?
Brokers (non-fiduciary)
- Must recommend “suitable” products, not necessarily best or least expensive
- Earn commissions or other transaction-based fees
- Must put clients interests before their own
- Most charge a fixed fee or percentage
A fiduciary duty is a legal and/or ethical relationship of confidence or trust between two or more parties. Typically, a fiduciary prudently takes care of money for another person. One party, for example a corporate trust company or the trust department of a bank, acts in a fiduciary capacity to the other one, who for example has funds entrusted to it for investment.
When a fiduciary duty is imposed, equity requires a different, arguably stricter, standard of behavior than the comparable tortious duty of care at common law. It is said the fiduciary has a duty not to be in a situation where personal interests and fiduciary duty conflict, a duty not to be in a situation where his fiduciary duty conflicts with another fiduciary duty, and a duty not to profit from his fiduciary position without knowledge and consent.
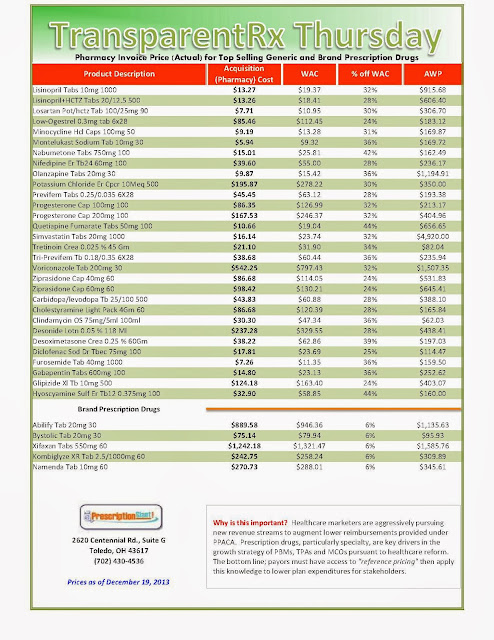
Resource for Payers: Acquisition Cost (pharmacy invoice) for Popular Brand & Generic Prescription Drugs
|
Include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to see if better pricing is available in the marketplace compared to what the client is currently receiving.
When better pricing is discovered the contract language should stipulate the client be indemnified. Do not allow the PBM to limit the market check language to a similar size client, benefit design and/or drug utilization. In this case, the market check language is effectually meaningless. |
Payers: Know Your Prescription Drug Opportunity Costs
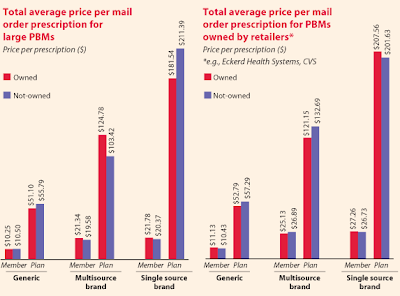
Excessive Mark-ups from Mail-order Prescriptions
It is not uncommon for some PBMs to mark-up mail-order medications as much as 500%! Why do you think traditional PBMs push so hard to move prescriptions to mail-order from retail?
A fiduciary PBM will not make an undisclosed profit from mail-order dispensed medications. Again, it will only charge its plan sponsor a flat administrative fee per claim unless some other arrangement has been agreed upon. The savings are passed back to plan sponsor reducing actual plan costs.
This is not to say that drugs dispensed via mail-order are a bad thing. In fact, mail-order can offer quite a bit of savings. But you must be aware of the arbitrage opportunities for non-fiduciary pharmacy benefits managers and eliminate them.


Again, if you don’t know the spread even exists or its amount how can a CFO or benefits director possibly determine the actual cost of the plan? This begs the question, “how does this happen?”
A simple example is when a PBM has different MAC price lists for plan sponsors and pharmacies. These MAC lists may differ in the number of drugs listed and/or their respective prices. A fiduciary PBM will not have any spreads and should contractually bound itself to such.
“Actual” Acquisition Costs (what pharmacy pays) of Top Selling Generic and Brand Prescription Drugs: for Payers
_1.jpg) |
||
As of 12/5/2013 – Published Weekly on Thursdays
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list. Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions. Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our pharmacy cost then determine if a problem exists. When there is a 10% or more price differential (paid versus actual cost) we consider this a problem. Multiple price differential discoveries means that your organization or client is likely overpaying. REPEAT these steps once per month.
|
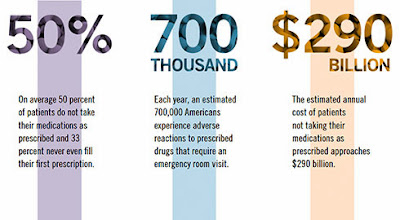
Some Patients Need Help with Medication Adherence from Pharmacists
Former Surgeon General C. Everett Koop once remarked, “Drugs don’t work in patients who don’t take them.”
These findings show that there are opportunities for prescription drug plans and policymakers to increase the nation’s overall adherence grade. On a federal level, NCPA urges Congress to pass the Medication Therapy Management Empowerment Act (S. 557 in the U.S. Senate and H.R. 1024 in the U.S. House of Representatives) to expand medication therapy management (MTM) services to Medicare Part D beneficiaries. This would not cost the government a dime; previous MTM programs have been shown to lower overall costs as increased pharmacist engagement with patients has avoided costlier health care treatments and procedures.
There is a vested interest for all to increase adherence rates in patients, and enacting the aforementioned changes will help to reach that goal. By implementing common-sense reforms, we can help improve the adherence grade. After all, when it comes to safe medication use, anything less than an “A” is unacceptable.
Hoey is CEO of the National Community Pharmacists Association. The research referred to was commissioned by NCPA as part of the association’s Pharmacists Advancing Medication Adherence (PAMA) initiative, which is sponsored by Pfizer, Merck, and Cardinal Health Foundation.

_1.jpg)

_1.jpg)

.png)