Tip of the Week: Pass-Through and Transparent PBM Business Models are Small Ideas (Re-run)
 |
| Click to Learn More |
 |
| Click to Learn More |
How many businesses do you know want to cut their revenues in half? That’s why traditional pharmacy benefit managers don’t offer a fiduciary standard and instead opt for hidden cash flow opportunities such as rebate masking. Want to learn more?
 “Thank you Tyrone. Nice job, good information.” David Stoots, AVP
“Thank you Tyrone. Nice job, good information.” David Stoots, AVP
A snapshot of what you will learn during this 30 minute webinar:
This document is updated weekly, but why is it important? Healthcare marketers are aggressively pursuing new revenue streams to augment lower reimbursements provided under PPACA. Prescription drugs, particularly specialty, are key drivers in the growth strategies of PBMs, TPAs, and MCOs pursuant to health care reform.
How to Determine if Your Company [or Client] is Overpaying
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is more than a 5% price differential for brand drugs or 25% (paid versus actual cost) for generic drugs we consider this a potential problem thus further investigation is warranted.
Multiple price differential discoveries mean that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
It is a myth that the Big 6 (ESI, CVS, Optum, Humana, MedImpact and Prime) offers better price savings just because of their size. The myth is often perpetuated by the old guard who for a long time have personally benefited from overpayments received from opaque PBM business practices. We can’t expect the old guard to bite the hand that feeds them, can we?
This document is updated weekly, but why is it important? Healthcare marketers are aggressively pursuing new revenue streams to augment lower reimbursements provided under PPACA. Prescription drugs, particularly specialty, are key drivers in the growth strategies of PBMs, TPAs, and MCOs pursuant to health care reform.
How to Determine if Your Company [or Client] is Overpaying
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is more than a 5% price differential for brand drugs or 25% (paid versus actual cost) for generic drugs we consider this a potential problem thus further investigation is warranted.
Multiple price differential discoveries mean that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
Ohio Attorney General Dave Yost is going after a $101 billion corporation that used $20 million in taxpayer money to hire a pharmacy benefits manager to provide services for Medicaid recipients that essentially already were covered by another PBM paid by the state.
 |
| Click to Get Started! |
In a deal reported by The Dispatch in October 2018 as part of its Side Effects series, Centene Corp’s Buckeye Community Health Plan hired two other Centene companies, Envolve and Health Net, to handle pharmacy benefits — even though Buckeye already had hired CVS Caremark as a pharmacy benefits manager.
Officials said at the time that the “administrator” and “manager” were paid for basically doing the same job. The duplication by Buckeye — one of five managed-care organizations hired by the state to deliver health-care services to the 3 million Ohioans on Medicaid — was the main reason it was charging the state more than twice the per-prescription costs of the other four, a state consultant found.
Tyrone’s Comments:
I’ve never personally had my identity or a very large sum of money stolen from me. But I’ve got to imagine it would feel a lot like how AG Yost feels. That’s not to say Centene is guilty. In fact, chances are Centene will not be held liable. The contract the state of Ohio signed I’m sure allowed for an artificially low administration fee (e.g. per claim, PEPM etc.) on the front-end leaving the PBM to generate its management fee however it saw fit. The trade off then is great optics but poor cost performance. How else is the PBM going to pay dividends or make payroll on an $1 per paid claim administrative fee? When your administrative fee is artificially too low, say less than $6 per paid claim, alarm bells should be going off in your head. There are self-funded employers who pay more annually to PBMs in management fees than the drugs actually cost. Don’t be one of those employers. Be better.
“Corporate greed has led Centene and its wholly owned subsidiaries to fleece taxpayers out of millions. This conspiracy to obtain Medicaid payments through deceptive means stops now,” Yost said in an emailed statement. “My office has worked tirelessly to untangle this complex scheme, and we are confident that Centene and its affiliates have materially breached their obligations both to the Department of Medicaid and the state of Ohio.”
This document is updated weekly, but why is it important? Healthcare marketers are aggressively pursuing new revenue streams to augment lower reimbursements provided under PPACA. Prescription drugs, particularly specialty, are key drivers in the growth strategies of PBMs, TPAs, and MCOs pursuant to health care reform.
How to Determine if Your Company [or Client] is Overpaying
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is more than a 5% price differential for brand drugs or 25% (paid versus actual cost) for generic drugs we consider this a potential problem thus further investigation is warranted.
Multiple price differential discoveries mean that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
This document is updated weekly, but why is it important? Healthcare marketers are aggressively pursuing new revenue streams to augment lower reimbursements provided under PPACA. Prescription drugs, particularly specialty, are key drivers in the growth strategies of PBMs, TPAs, and MCOs pursuant to health care reform.
How to Determine if Your Company [or Client] is Overpaying
Step #1: Obtain a price list for generic prescription drugs from your broker, TPA, ASO or PBM every month.
Step #2: In addition, request an electronic copy of all your prescription transactions (claims) for the billing cycle which coincides with the date of your price list.
Step #3: Compare approximately 10 to 20 prescription claims against the price list to confirm contract agreement. It’s impractical to verify all claims, but 10 is a sample size large enough to extract some good assumptions.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is more than a 5% price differential for brand drugs or 25% (paid versus actual cost) for generic drugs we consider this a potential problem thus further investigation is warranted.
Multiple price differential discoveries mean that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
Always include a semi-annual market check in your PBM contract language. Market checks provide each payer the ability, during the contract, to determine if better pricing is available in the marketplace compared to what the client is currently receiving.
 |
| Click to Learn More |
Humana Inc. has agreed to join a purchasing group run by rival Cigna Corp. in a move that the health insurer says will help drive down its drug costs for its commercial members. Beginning April 1, Humana will join a Cigna purchasing organization called Ascent Health Services to give it access to greater discounts from drugmakers, the companies confirmed to Bloomberg News. Ascent manages commercial rebates, the payments that drugmakers make to health plans. The agreement covers drug contracting and negotiations for Humana’s commercial business.
“This arrangement will help us leverage scale and buying power to extract deeper price discounts from drug manufacturers and advance affordability for our customers while at the same time preserve our ability to address their specific clinical needs,” Humana spokeswoman Kelley M. Murphy said in an email.
Tyrone’s Commentary:
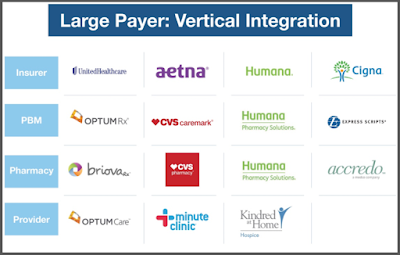
This move and others like it are a play to hold on to the undisclosed cash flows non-fiduciary PBMs generate from drug manufacturers for rebates. In place of rebate disguising, non-fiduciary PBMs charge manufacturers fees as part of the GPO or group purchasing organization. This arrangement technically (by passing through all manufacturer revenue less GPO fees to plan sponsors) allows non-fiduciary PBMs to be in compliance with the new regulations being placed on us by departments of insurance across the country. Radical transparency requires that plan sponsors are able to verify the fees earned by PBMs in these GPO arrangements.
Cigna and Humana both sell health insurance and other medical services, including pharmacy benefits. Cigna has expanded its footprint in the pharmacy business since its 2018 acquisition of Express Scripts. In 2019, Cigna announced a three-year deal to work with Prime Therapeutics LLC, a pharmacy-benefit manager owned by Blue Cross and Blue Shield plans. Cigna executives have described how working with outside partners like Prime can increase purchasing leverage with drugmakers.