Reviewing PBM Alternative Pricing Models for CVS Health, ESI, and OptumRx [Weekly Roundup]
Reviewing PBM Alternative Pricing Models for CVS Health, ESI, and OptumRx and other notes from around the interweb:
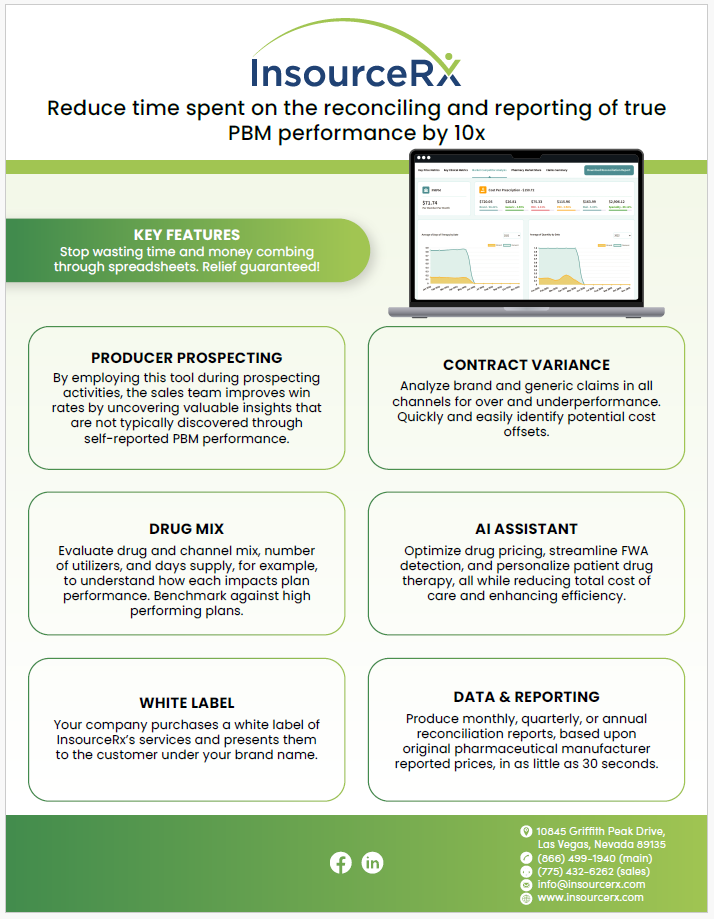
- Reviewing PBM Alternative Pricing Models For CVS Health, ESI, and OptumRx. PBM alternative pricing models are being rolled out by some of the biggest organizations in the industry in response to mounting political pressure, changing legislation, and the prevalence of industry disruptors. PSG has closely assessed the strategies put forward by CVS Health, ESI, and OptumRx regarding pharmacy reimbursement and client pricing models. We will take a deeper look at network contracting strategies like CVS CostVantage and ESI ClearNetwork in addition to client pricing strategies such as CVS Caremark TrueCost, ESI ClearCareRx, OptumRx Cost Advantage, and OptumRx Cost Clarity and share some considerations for how plan sponsors should address the changing pricing landscape.
- GLPs Are the Latest Example of the Shift to Alternative Purchasing Models. Prior to the rollout of Medicare Part D in 2006, the Medicare population represented the largest out-of-pocket consumer group in the cash pay marketplace. Then it was the uninsured prior to the Affordable Care Act (ACA). Then, after the ACA exchanges and Medicaid expansion, the cash pay strategy turned to middle- and upper middle–class households, with the fewest regulatory restrictions, the most disposable income, and, importantly, the highest deductibles for drug coverage. Many of these individuals had to spend many thousands of dollars for first dollar coverage. A large swath of the American population has now become accustomed to not even bothering with their pharmacy benefit manager (PBM), and the first question that comes to mind isn’t “Does my insurance cover it?” but rather, “What’s the easiest and most convenient way for me to get a prescription for the drug I saw on my social media feed?”
- Explainer: Why are US pharmacy benefit managers under fire? Separate bills aim to ban what is known as “spread pricing,” a practice in which PBMs charge health plans a larger amount for a drug than they pay out to pharmacies. Some are seeking more transparency under which the companies would be required to provide more information on their non-public negotiations. Rebates have also been a subject of proposed new government rules. The Trump administration sought in 2020 to make rebates illegal for Medicare prescription drug plans by removing the safe harbor protection that shields rebates from federal anti-kickback laws. The Biden administration delayed the rule until 2023 and Congress further delayed it until 2027.
- How GoodRx Helped Steal $7 From My Pharmacy. GoodRx, primarily known as a platform for obtaining prescription coupons and tracking drug prices, interacts with Pharmacy Benefits Managers (PBMs) in a way that’s distinct from traditional PBM operations. In essence, GoodRx leverages the existing PBM infrastructure to provide discounted prices directly to consumers, often bypassing the more traditional insurance-based prescription purchasing pathway. For benefits consultants and employers, understanding this interaction is crucial in advising on healthcare strategies that maximize both cost efficiency and patient outcomes. Employers need to consider how tools like GoodRx fit into a broader benefits design, particularly in terms of how they affect out-of-pocket costs for employees and the overall usage of pharmacy benefits managed under traditional PBM contracts.