I’m Worried! Triple Agonist GLP-1 Retatrutide is on the Way
In the ever-evolving landscape of pharmacy benefit management, few developments have stirred as much excitement—and anxiety—as the introduction of triple agonist GLP-1 Retatrutide. With the potential to revolutionize treatments for diabetes and obesity, this novel drug is making waves. But what exactly is an agonist, and why is Retatrutide causing such a stir?
Understanding Agonists
First, let’s break down what an agonist is. In pharmacology, an agonist is a substance that binds to a specific receptor on a cell and triggers a response, mimicking the action of a naturally occurring substance. Think of it like a key fitting into a lock and turning it. When the key (agonist) binds to the lock (receptor), it opens the door (activates the receptor) to produce a specific effect.
Zepbound, Mounjaro, Wegovy, and Ozempic all function by reducing appetite, but there are key differences in their mechanism of action. Zepbound and Mounjaro are known as “dual-agonist” drugs, while Wegovy and Ozempic are “single-agonist” drugs. These medications activate essential hormone pathways in the body to achieve their effects.
What Makes Retatrutide Special?
Retatrutide stands out because it is a triple agonist. This means it simultaneously activates three different types of receptors:
- GLP-1 Receptor (Glucagon-Like Peptide-1)
- GIP Receptor (Glucose-Dependent Insulinotropic Polypeptide)
- Glucagon Receptor
By targeting these three receptors, Retatrutide offers a multifaceted approach to managing blood glucose levels, enhancing insulin secretion, and potentially promoting weight loss. This multi-receptor activation could provide superior efficacy compared to current single or dual agonist therapies. Enrollees in the clinical trial receiving Retatrutide also experienced improvements in blood pressure and lipid profile.
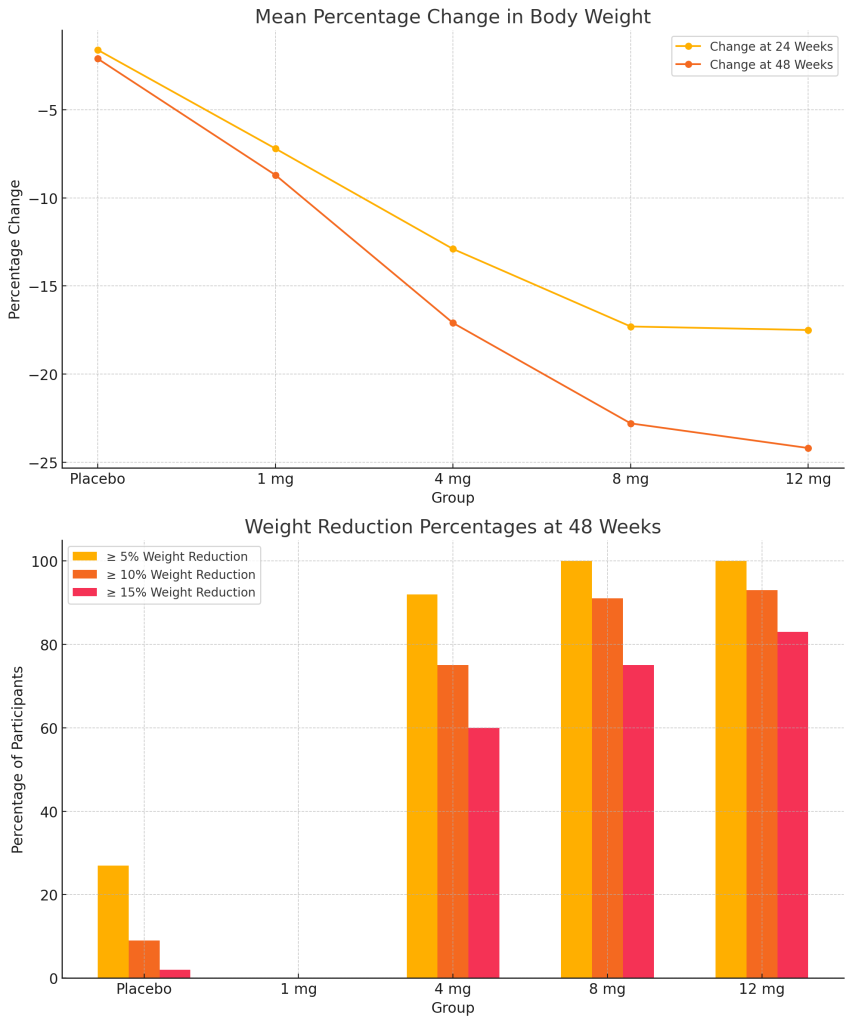
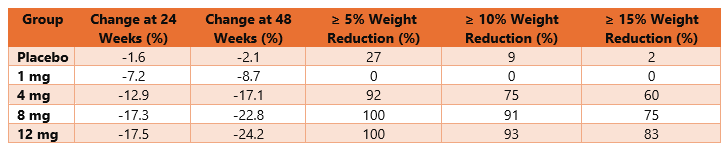
Here are the detailed results from the Retatrutide study:
Key Observations
- Change in Body Weight: The graphs above illustrate the mean percentage change in body weight at 24 and 48 weeks across different dosage groups, highlighting the significant impact of Retatrutide on weight reduction compared to placebo.
- Weight Reduction Percentages: The bar chart shows the percentage of participants achieving weight reductions of 5%, 10%, and 15% or more at 48 weeks.
The Promise of Retatrutide
- Improved Glycemic Control: By activating the GLP-1 and GIP receptors, Retatrutide can significantly enhance insulin secretion in response to meals, leading to better blood sugar control.
- Weight Management: The activation of these receptors also influences appetite regulation and energy expenditure, potentially aiding in substantial weight loss for individuals with obesity.
- Cardiovascular Benefits: Preliminary studies suggest that Retatrutide may offer cardiovascular benefits, reducing risks associated with diabetes and obesity.
Why Worry?
Despite the promising benefits, the introduction of Retatrutide is not without concerns:
- Side Effects: As with any new medication, there are potential side effects. These could range from gastrointestinal issues to more serious concerns that have yet to be fully understood.
- Long-term Safety: The long-term effects of triple receptor activation are still under investigation. It’s crucial to ensure that the benefits outweigh the risks over extended use.
- Cost and Accessibility: New drugs often come with high price tags, and access can be limited by insurance coverage and healthcare policies. Ensuring that those who need Retatrutide can afford it will be a significant challenge.
Conclusion
As a new pharmaceutical sales rep at Eli Lilly, I toured the manufacturing facility for Cialis. The experience was astounding; advanced robotics handled every step of production, from mixing raw ingredients to pressing and packaging tablets, all without human interaction. Hundreds of tablets were manufactured every minute, a testament to the incredible advancements in pharmaceutical manufacturing technology.
Fast forward to today, and I see the same excitement and potential in the pending launch of Retatrutide. Just as those robotics revolutionized Cialis production, Retatrutide promises to revolutionize the treatment of diabetes and obesity with its triple-agonist approach. However, the cost implications cannot be ignored.
Self-funded employers, already navigating the complexities of healthcare costs, now face the challenge of incorporating this expensive but potentially life-changing medication into their plans. While the potential health benefits of Retatrutide are immense, it is crucial to balance these benefits with the financial realities.
Employers must consider strategies to manage these costs effectively, ensuring that they can provide the best care for their employees without compromising their financial stability. My best advice to you is pick the right pharmacy benefit manager.