Eight Reasons Employers Overpay For PBM Services
7. Lack of Accountability – Usually it is a cross-functional team which agrees upon a pharmacy benefits management provider. In my opinion, this sort of consensus building is the correct approach but may ultimately lead to passing the buck. If things go south who takes responsibility and rights the ship? Typically, no one thus the overpayments or poor service problems fester for years.
6. Macro approach rather than Micro – Employers don’t evaluate at the micro level or intensely supervise PBMs. As a result, they leave themselves open for excessive overpayments. In the words of Ronald Reagan, “Trust but Verify.”
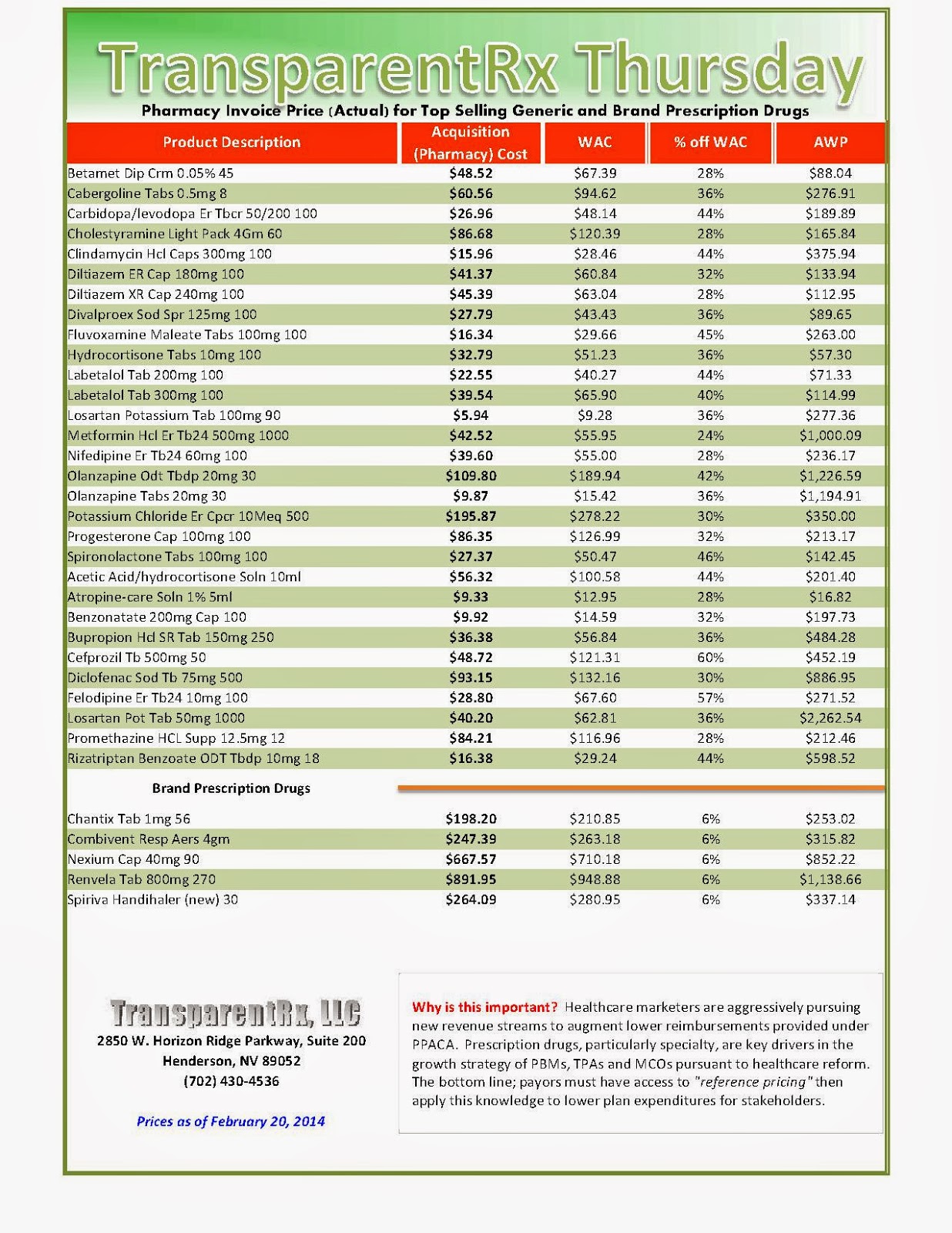
5. Hired the Wrong PBM – Traditional PBMs profit from overpayments. These hidden costs are typically extracted from spreads, manufacturer revenue (more than just rebates) and dispensing fees. Fiduciary PBMs, on the other hand, profit from only an administration fee whether PMPM or per claim. True transparency leads to a reduction of overall plan costs.
 4. Hired the Wrong Consultant or Broker – This scenario plays out year after year…a self-insured employer hires a large benefits consultant firm to manage the RFP process. The employer thinks great we receive all this expertise at little to no cost. There are two problems here: 1) benefits consultants are not necessarily experts in the PBM industry. In fact, they often know little more than the employer 2) the benefits consultant will, based upon an agreement with the PBM, TPA or ASO, select and/or recommend the bid which provides it the most fees. Experts utilize their knowledge, skills and resources to generate extraordinary results not psychobabble.
4. Hired the Wrong Consultant or Broker – This scenario plays out year after year…a self-insured employer hires a large benefits consultant firm to manage the RFP process. The employer thinks great we receive all this expertise at little to no cost. There are two problems here: 1) benefits consultants are not necessarily experts in the PBM industry. In fact, they often know little more than the employer 2) the benefits consultant will, based upon an agreement with the PBM, TPA or ASO, select and/or recommend the bid which provides it the most fees. Experts utilize their knowledge, skills and resources to generate extraordinary results not psychobabble. 1. Ignorance – Defined in the Merriam-Webster dictionary as lacking knowledge or comprehension of the thing specified; unaware or uninformed. When dealing with PBMs it’s not what you know, but instead what you don’t know that subjects plan sponsors to excessive overpayments.
Click here to register for: “How To Slash the Cost of Your PBM Service, up to 50%, Without Changing Providers or Employee Benefit Levels.”
_1.jpg)

_1.jpg)
_1.jpg)
_1.jpg)
_1.jpg)