In the realm of employee health and wellness, medication adherence plays a pivotal role in managing chronic conditions and reducing healthcare costs. For Chief Human Resources Officers (CHROs) and Chief Financial Officers (CFOs), ensuring high medication adherence rates among employees is not just a matter of health but also impacts the bottom line. This is where Advanced Pharmacy Benefit Management (PBM) steps in, offering strategic solutions to enhance medication adherence and optimize healthcare expenditures. Now, let’s explore how advanced PBM strategies can assist HR and finance leaders in improving medication adherence among employees:
- Data-Driven Insights: Advanced PBMs leverage data analytics to identify trends and patterns in medication adherence among employee populations. By gaining insights into adherence behaviors, CHROs and CFOs can tailor targeted interventions and wellness programs to address specific adherence challenges within their workforce.
- Cost-Effective Benefit Design: PBMs work closely with employers to design prescription benefit plans that incentivize medication adherence while managing costs effectively. Through strategies such as value-based formularies and patient-centric utilization management programs, CHROs and CFOs can optimize medication access while containing healthcare expenditures.
- Healthcare Navigation Services: Some advanced PBMs offer healthcare navigation services to guide employees through their medication journey, from prescription initiation to refill management. By providing personalized support and resources, HR and finance leaders can empower employees to make informed decisions about their health and medication regimens.
- Financial Impact Analysis: PBMs provide CHROs and CFOs with comprehensive reporting and analytics tools to assess the financial impact of medication adherence on overall healthcare spending. By quantifying the cost savings associated with improved adherence, HR and finance leaders can demonstrate the value of investing in adherence-enhancing initiatives.
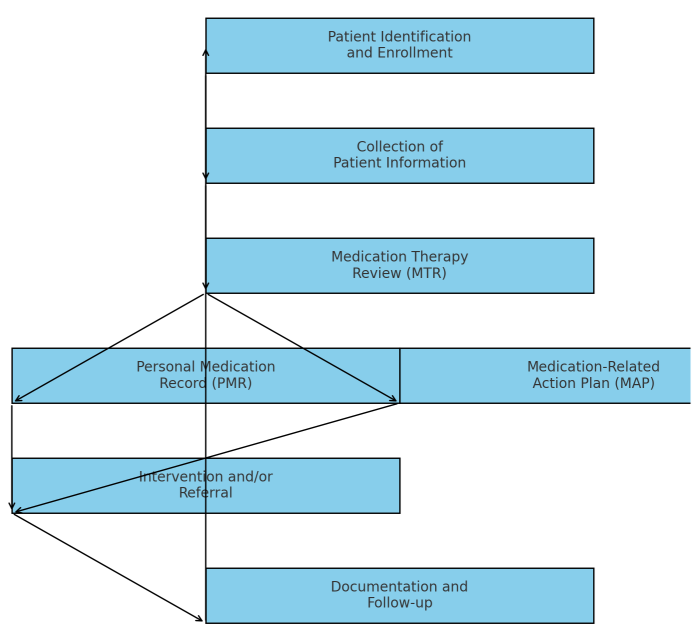
- Medication Therapy Management (MTM): This service involves personalized medication reviews and consultations conducted by pharmacists to optimize medication regimens, improve adherence, and minimize adverse effects. By engaging employees in one-on-one discussions about their medications, HR and finance leaders can enhance medication understanding and compliance.
- Proportion Days Covered and Medication Possession Ratio: These metrics quantify medication adherence by assessing the percentage of time employees have access to their prescribed medications. Proportion Days Covered (PDC) measures the duration of medication supply coverage over a specific period, while Medication Possession Ratio (MPR) calculates the ratio of days medication is on hand compared to the total days in a set timeframe. By monitoring these metrics, HR and finance leaders can gauge the effectiveness of adherence initiatives and identify areas for improvement in employee health management strategies.
In summary, optimizing medication adherence through advanced Pharmacy Benefit Management is not only a strategic imperative for improving employee health outcomes but also a prudent financial decision for organizations. By leveraging data-driven insights, cost-effective benefit design, and personalized support services, CHROs and CFOs can drive positive health outcomes while maximizing the return on investment in employee healthcare benefits.