 |
| Radical transparency in pharmacy benefits management starts with training and education. Click here to begin yours. |
If a PBM does not get on a plan’s formulary, the manufacturer loses sales and market share. The Data show that manufacturers need not provide much of a rebate for drugs that are still on patent and have few rivals, but they tend to give larger rebates when they have less leverage in negotiations regarding drugs with several possible substitutes–either generics or simply drugs with comparable effects.
These rebates are tantamount to discounts off the drug manufacturer’s list price. PBMs do not keep the entire rebate that they negotiate: The lion’s share goes to insurers, which allows them to keep premiums lower.
Tyrone’s Commentary:
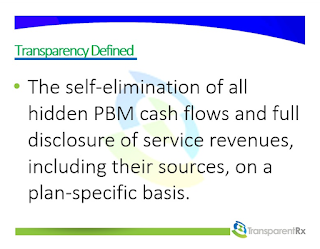
It’s true rebates can reduce net prices. The burden, however, is on self-insured employers to extract those rebate dollars from the PBM and to not allow the non-fiduciary PBM to profit from manufacturer revenue or rebates. Because they tend to be more sophisticated purchasers, insurers are better at keeping rebate dollars than are self-insured employers. How well a PBM performs depends largely on the sophistication level of their clients. If the self-insured employer is unsophisticated, the non-fiduciary PBM and any benefits consultant whose interests are misaligned will feast off hidden cash flow. These cash flows are hidden in the employers’ final plan costs thus equate to a service.
[Read More]