 |
| Figure 1 |
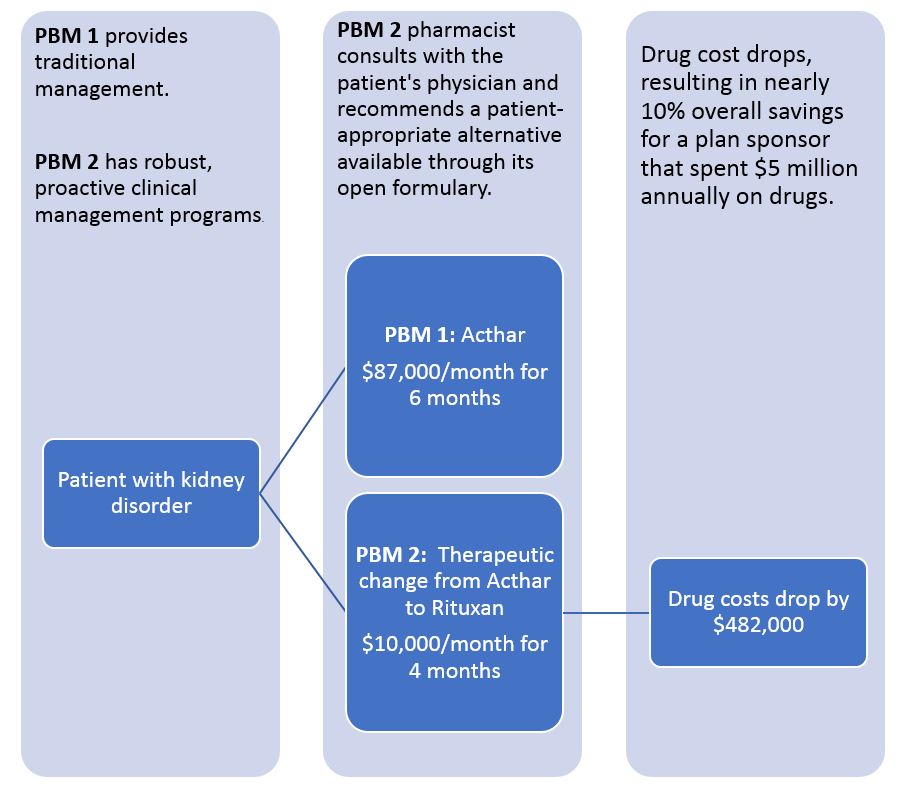
For many health benefit plan sponsors and their advisors, the evaluation process used to compare pharmacy benefits managers (PBMs) keeps drug costs higher than they should be by measuring their value with metrics that reward rebates rather than net costs.
For example (see Figure 1), a patient with nephrotic syndrome is part of a real-world, self-funded drug plan that switched from PBM 1 to PBM 2. If presented with this scenario during an RFP analysis, is your evaluation process set up to value the larger rebate associated with Acthar, or the overall lower costs associated with Rituxan?
Tyrone’s Commentary:
When monitoring PBM performance during the contract term, go beyond standard reports. These reports don’t usually uncover problem areas that if resolved cuts the PBM’s service fee but saves you [plan sponsor] money. How do you go beyond standard reports you might ask? For starters, download a copy of my 18 pt. PBM Performance Evaluation Questionnaire. Work with the PBM account manager on a corrective action plan when problems are uncovered. Some problems might include:
1. MAC list performance
2. Performance guarantee true ups
3. PA and ST rubber-stamping
4. Poor product mix
5. Improper utilization
An RFP process that “spreadsheets” acquisition discounts, rebates per prescription, and administration costs typically lacks the information that plan sponsors need to recommend the option with the lowest overall costs and doesn’t account for utilization management or improved clinical outcomes.