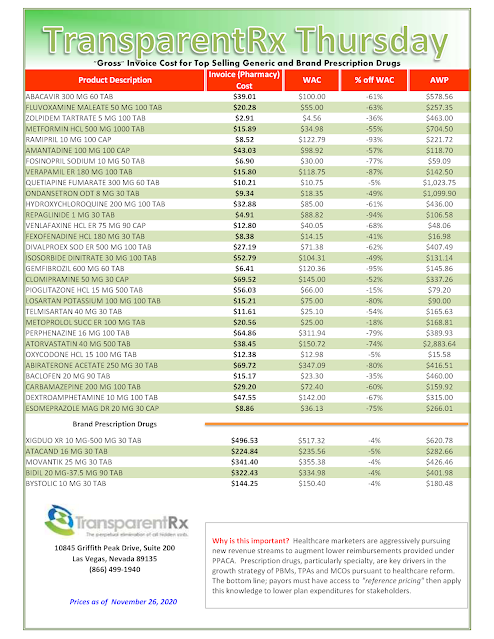
Reference Pricing: “Gross” Invoice Cost vs. AWP for Popular Generic and Brand Prescription Drugs (Volume 342)
This document is updated weekly, but why is it important? Healthcare marketers are aggressively pursuing new revenue streams to augment lower reimbursements provided under PPACA. Prescription drugs, particularly specialty, are key drivers in the growth strategies of PBMs, TPAs, and MCOs pursuant to health care reform.
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is more than a 5% price differential for brand drugs or 25% (paid versus actual cost) for generic drugs we consider this a potential problem thus further investigation is warranted.
Multiple price differential discoveries mean that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
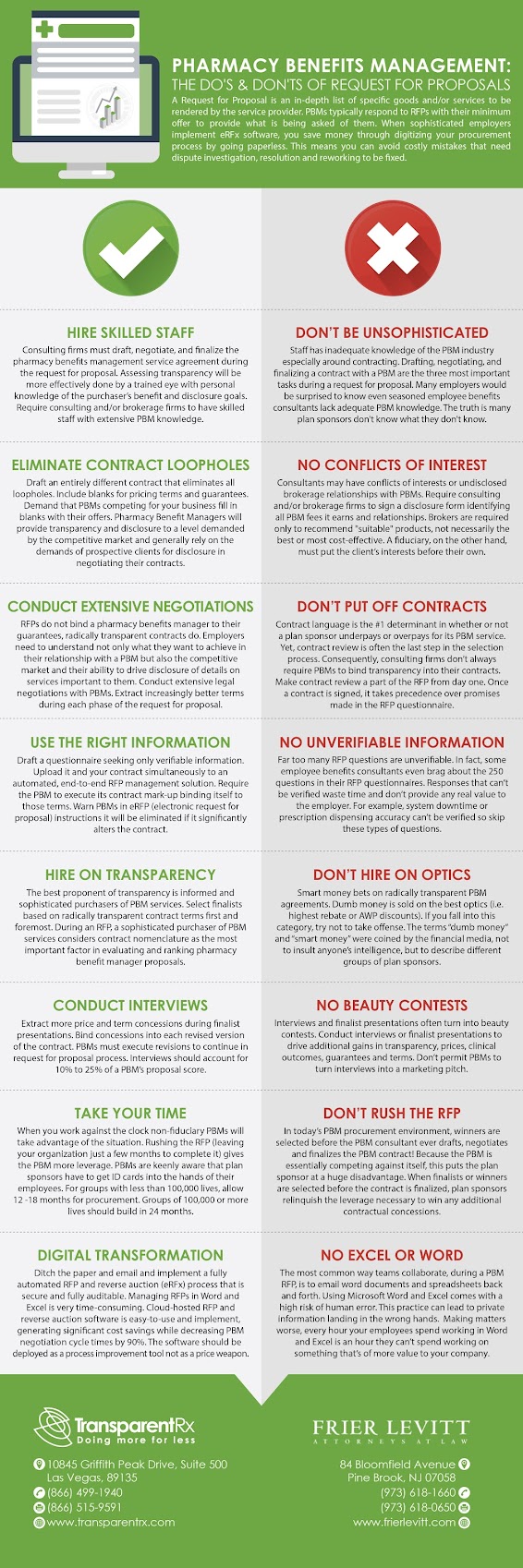
Tuesday Tip of the Week: 3 Ways for Employers and HR Pros to Know If They Have Selected the Right Insurance Broker for Pharmacy Benefits
About 15% of employers change brokers each year and likely double that stay with their broker even though they are not satisfied with the ROI. At the point when you consider the effect of the Covid-19 pandemic on staff, HR groups need now, like never before, to know their employee benefit brokers are genuine advocates and fully aligned in accomplishing HR goals. Here are three tips for employers and HR professionals to help pick the right insurance broker for pharmacy benefits.
1. Broker relies on technology.
2. Ask about conflict of interests.
If you’re reading this and work in HR or finance for a self-funded employer, never retain the services of a broker or PBM consultant who benefits when your pharmacy costs increase. Should you do so, be sure to have signed a conflict of interest disclosure form.
- Do you have the expertise within your company to evaluate PBM contract language?
- Do you have the skillset to design a pharmacy benefit plan? Or do you need additional training in pharmacy benefits management?
- Do you have the expertise and resources to manage the plan design or do you need to build in the incentives for the PBM to manage your program?
- How do you want to be involved in the management of the plan after it is set up?
A potential or actual conflict of interest exists when commitments and obligations are likely to be compromised by the broker’s other material interests, or relationships (especially economic), particularly if those interests or commitments are not disclosed. In other words, hire consultants not because you lack the requisite knowledge to design or manage the pharmacy benefit plan in-house, but because you lack the time or human capital to go it alone.
 |
| Find Out More |
3. Check the credentials.
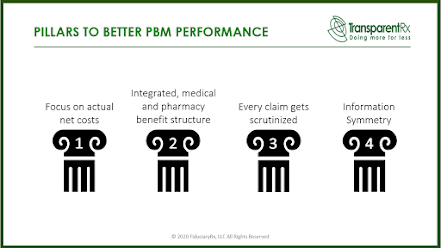
Many employers, unions, and government agencies pay large consultancies and brokerage firms to help them avoid overpaying for pharmacy services. So then how does this keep happening? There are a number of reasons including misaligned incentives, inefficient procurement and overall lack of a pharmacy benefits strategy just to name a few. But, the primary reason is without question a wholesale lack of education around pharmacy benefits management in general. It is education which leads employers to leveraging the four pillars to better PBM performance. When you hear an insurance broker say, “I know just enough about pharmacy benefits to be dangerous” run for the hills!
Education is key to use of lowest net cost drugs in pharmacy benefit plans. Only the most sophisticated purchasers of PBM services will have the knowledge and confidence to bind lowest net costs for prescription drugs into contract language and benefit design. Hence, your competitive advantage includes executing good analysis of the correct information then deciding what all of this suggests for your organization. Those who seize the chance and develop a good plan that may reasonably be accomplished have a higher probability of getting to lowest net cost.
Ohio Requesting Bids for Administrator to Oversee its Pharmacy Benefit Program
The Ohio Department of Medicaid on Thursday started the process of hiring a private administrator to oversee its $3 billion pharmacy benefit program. The department requested proposals for a pharmacy operational support vendor to help design its program and provide financial oversight once it’s up and running. Medicaid created the new post as part of a broader overhaul of its managed care program.
 |
| Find Out More |
In addition to rebidding contracts with private managed care organizations that oversee the program, the state agency is also replacing five pharmacy benefit managers hired by those private organizations to process claims with one company hired by the state and monitored by the administrator. The added oversight comes after a report showed PBMs billed the state far more than they paid pharmacists and kept the difference, allowing them to receive $224 million in one year — an amount generated by PBMs charging three to six times the standard rate, according to an independent analysis.
Tyrone’s Commentary:
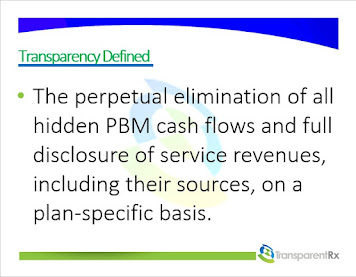
Your pharmacy benefit manager owes you nothing. In its most simplistic form it is merely a facilitator of goods and services. At best, it is your adviser offering suitable goods and services but not necessarily the best goods or services. To owe its client something, the PBM would have to act as a fiduciary. Have you noticed how often PBMs get sued but rarely lose in court? Employers believe that PBMs owe it something the courts say otherwise. You see non-fiduciary PBMs generally rely on the demands of its clients for how much cost savings they will provide. Moreover, non-fiduciary PBMs provide disclosure of important contract details to a level demanded by the competitive market. In other words, non-fiduciary PBMs have learned how to leverage the purchasing power of the unsophisticated plan sponsor to their financial advantage. The truth is most, if not all, of the excessive costs embedded in non-fiduciary PBM service agreements can be eliminated if stakeholders (HR execs, CFOs, benefits consultants, brokers etc…) concern themselves more with self-education and accountability and less with self-preservation. If I here one more time “no one has ever been fired for hiring Express Scripts”😕. The state of Ohio was humbled and now has a plan to win full disclosure and eliminate overpayments to non-fiduciary PBMs. You could establish a POSV or just hire a fiduciary-model PBM and achieve two aims at once – eliminate PBM overpayments and do away with duplicative consulting fees. What is your pharmacy benefits management strategy?
“The POSV (pharmacy operational support vendor) will ensure monetary incentives are properly and fairly aligned, eliminate self-dealing and steering, and monitor and close potential pricing or rebate loopholes,” said Medicaid Director Maureen Corcoran. “In short, the POSV ensures that the fox is no longer guarding the chicken coop.” The administer will operate independently from the pharmacy benefit manager, providing oversight and ensuring pharmacists are paid accurately for the prescriptions they fill.
[Free Webinar] The Untold Truth: How Pharmacy Benefit Managers Make Money
“Thank you! Awesome presentation.” Mallory Nelson, PharmD
“Thank you Tyrone for this informative meeting.” David Wachtel, VP
“…Great presentation! I had our two partners on the presentation as well. Very informative.” Nolan Waterfall, Agent/Benefits Specialist
A snapshot of what you will learn during this 30-minute webinar:
- Hidden cash flow streams in the PBM Industry
- Basic to intermediate level PBM terminologies
- Examples of drugs that you might be covering that are costing you
- The #1 metric to measure when evaluating PBM proposals
- Strategies to significantly reduce costs and improve member health
Sincerely,
TransparentRx
Tyrone D. Squires, MBA
10845 Griffith Peak Drive, Suite 200
Las Vegas, NV 89135
866-499-1940 Ext. 201
P.S. Yes, it’s recorded. I know you’re busy…so register now and we’ll send you the link to the session recording as soon as it’s ready.
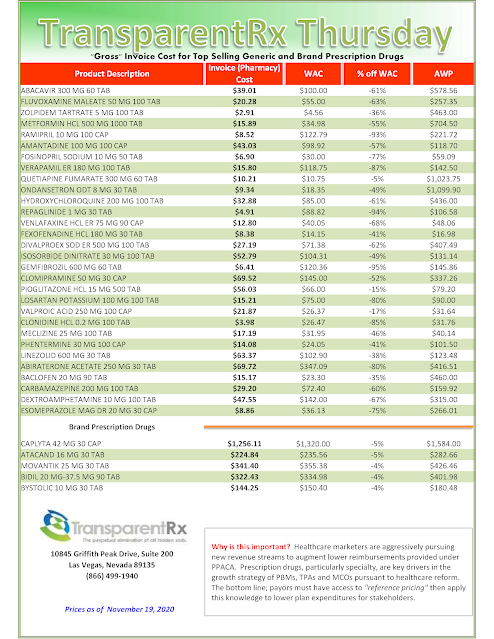
Reference Pricing: “Gross” Invoice Cost vs. AWP for Popular Generic and Brand Prescription Drugs (Volume 341)
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is more than a 5% price differential for brand drugs or 25% (paid versus actual cost) for generic drugs we consider this a potential problem thus further investigation is warranted.
Multiple price differential discoveries mean that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —
Tuesday Tip of the Week: Non-Fiduciary PBM Rent-Seeking Behavior Eliminates Their Price Advantage
Rent-seeking is a term economists use to describe an organization’s ability to generate above average economic returns without providing any relative incremental value. Wikipedia may explain it a bit better.
Wikipedia Definition
The simplest definition of rent-seeking is to expend resources in order to gain wealth by increasing one’s share of currently existing wealth instead of trying to create wealth. Since resources are expended but no new wealth is created, the net effect of rent-seeking is to reduce total social wealth. It is important to distinguish between profit-seeking and rent-seeking.
Profit-seeking is the creation of wealth, while rent-seeking is the use of social institutions such as the power of government to redistribute wealth among different groups without creating new wealth. Rent-seeking generally implies extraction of uncompensated value from others without making any contribution to productivity.
Studies of rent-seeking focus on efforts to capture special monopoly privileges such as manipulating government regulation of free enterprise competition. The term monopoly privilege rent-seeking is an often-used label for this particular type of rent-seeking. Often-cited examples include a lobby that seeks tariff protection, quotas, subsidies, or extension of copyright law.
Reference Pricing: “Gross” Invoice Cost vs. AWP for Popular Generic and Brand Prescription Drugs (Volume 340)
Step #4: Now take it one step further. Check what your organization has paid, for prescription drugs, against our acquisition costs then determine if a problem exists. When there is more than a 5% price differential for brand drugs or 25% (paid versus actual cost) for generic drugs we consider this a potential problem thus further investigation is warranted.
Multiple price differential discoveries mean that your organization or client is likely overpaying. REPEAT these steps once per month.
— Tip —